Is tinea capitis improved in children?
summary
Clinically, for patients with tinea capitis, the occurrence of this disease has a great impact on the patients. Therefore, when patients find the symptoms of tinea capitis, they must go to the hospital as soon as possible to check the situation of tinea capitis. If patients are treated with tinea capitis, they should not only actively cooperate with the doctor's treatment plan for tinea capitis, But also to adhere to the scientific nursing of tinea capitis, in order to promote the rehabilitation of tinea capitis. So children tinea capitis improvement symptom? Now let's make a specific analysis.
Is tinea capitis improved in children?
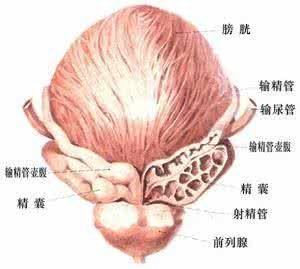
1. Tinea favosa mainly occurs in children, adults and adolescents. At the beginning of the red spots, scalp inflamed red, and there are thin flakes of scale, after that, the formation of hair as the center of the dish shaped yellow scab, known as the Yellow scab. There are a lot of ringworm around the hair follicle mouth of the affected area, and there are hairs running through the middle. The scab was peeled off, and the red slightly concave erosive surface was under it. The scab of tinea flava gradually expanded and fused to form a large dirty scab, often accompanied by rat odor. In the affected area, the hair is dark and lusterless, but seldom broken. Long term patients, hair follicles atrophy, hair loss, the formation of large permanent alopecia. Normal hair may remain in the center of the scalp, and the hairline area around the scalp is usually not involved. Patients generally have no obvious symptoms or mild itching. Secondary infection may be accompanied by fever and local lymphadenopathy. Some patients only showed seborrheic dermatitis without typical tinea flava scab, which is easy to be misdiagnosed.

2. Psoriasis capitis is a common disease in children, especially in preschool children. In the early stage, the lesions on the head are grayish white scaly patches (Fig. 14-2), round or oval, and then one or several smaller similar lesions may appear nearby. The hair in the affected area is usually broken 2-4mm away from the scalp, with white bacterial sheath around it, which is due to the formation of fungal spores parasitizing outside the hair. Broken hair is easy to pull out. Generally no symptoms, occasionally mild itching. Psoriasis after puberty due to increased sebum secretion of hair, containing unsaturated fatty acids inhibit the pathogenic fungi, can also be self-healing, after healing does not leave scars. Most of them are caused by microsporium laniformis or microsporium ferrugosum. Incidence rate of primary school is mainly due to the increase of the number of cats and dogs in the city. At the beginning of the disease, it was a white scaly limited patch with a slight itching sensation and a clear boundary. There was a white sheath like fungus at the root of the disease, and there was a broken hair about 0b5cm away from the scalp. Puberty can be self-healing, this may be due to puberty sebaceous glands developed, scalp free fatty acids have a certain inhibitory effect on fungi. There is no scar after healing.

3. The pathogenic bacteria of tinea nigra are tinea purpurea or tinea interrupted. The symptoms are an inflammatory papule at the root of the hair, which is the size of beans or nails, with reddish spots or bald spots. Some of them have a thin layer of shavings. Hair is easy to break off from the root, showing black spots, easy to pull out without pain. The disease can occur in both urban and rural areas. First of all, we should pay attention to the prevention work. The sick children's hats, pillows, combs and hairdressing appliances must be strictly disinfected. They can be soaked in 5% Lysol or 5% formalin for 15-20 minutes.

matters needing attention
(1) patients' clothes, hats and pillows should be sun dried, scalded and boiled for disinfection; Contaminated hairdressing tools should be brushed, washed and soaked; The hair, scales and scab with bacteria should be burned; Don't wear hats, towels, etc. (2) griseofulvin should be taken continuously for four weeks. At the same time, 5% sulfur ointment, 2% iodine tincture or other antifungal drugs should be used externally. If the bacteria were negative after 4 weeks and normal new hair grew, the drug can be stopped. Because of the side effects of griseofulvin, such as nausea, headache, photosensitive rash, occasional leukopenia, positive urine protein, abnormal liver function of some patients, we should pay attention to the time and dose of medication. (3) ketoconazole has some side effects on liver, so it is necessary to check liver function regularly. (4) artificial hair removal treatment: for small area, this treatment can be considered. Remove the diseased hair with forceps, and then use 2% iodine tincture.